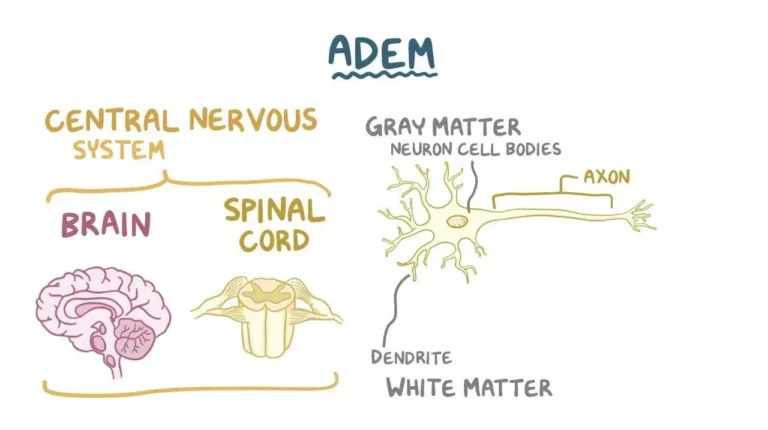
Acute disseminated encephalomyelitis (ADEM) is a rare, immune-mediated inflammatory disorder that affects the brain and spinal cord. It most often follows a recent infection and, far less commonly, can occur after vaccination; in some cases, no clear trigger is found. ADEM is typically monophasic (a single attack) and has an abrupt onset.
Key Points
- Usually occurs 1–3 weeks after a viral or bacterial illness.
- Most common in children and young adults, but it can occur at any age.
- Early recognition and treatment improve outcomes.
What Happens in ADEM?
In ADEM, the immune system mistakenly attacks the protective myelin sheath around nerve fibers, leading to widespread (disseminated) inflammation, especially in the brain’s white matter. This disrupts normal nerve signaling and causes neurological symptoms.
Common Symptoms
Symptoms tend to start suddenly and evolve over hours to days. They may include:
- Fever, headache, profound fatigue, and altered alertness (confusion, drowsiness).
- Neurological deficits: weakness or numbness in an arm/leg, balance or coordination problems, visual changes, speech difficulties.
- Seizures (in some patients); severe cases can progress to coma without prompt care.
While early symptoms can be mild, ADEM can deteriorate rapidly. Urgent medical evaluation is crucial if new neurological symptoms appear, especially after a recent infection.
Who Is at Risk?
ADEM can affect anyone, but it is reported more frequently in children and adolescents. Many patients have had a recent respiratory or gastrointestinal illness. Post-vaccination ADEM is very rare; overall, the health benefits of vaccination far outweigh this small risk.
How Is ADEM Diagnosed?
Diagnosis is clinical and supported by tests that help rule out infections and other conditions:
- MRI of the brain/spinal cord typically shows multiple inflammatory lesions, often in the white matter.
- Spinal fluid (lumbar puncture) may show mild inflammation and helps exclude infections.
- Blood tests and, when needed, additional studies help distinguish ADEM from other disorders (for example, multiple sclerosis).
Treatment
The first-line therapy is usually high-dose corticosteroids to reduce inflammation. If there is an inadequate response or contraindications, doctors may consider intravenous immunoglobulin (IVIG) or plasma exchange. Supportive care—sometimes in an intensive care unit—is provided as needed to manage seizures, breathing problems, or significant weakness.
Recovery & Outlook
With prompt treatment, many patients—especially children—recover fully over weeks to months. Some may have lingering issues such as fatigue, attention difficulties, or mild motor/vision problems. Recurrence is uncommon, but follow-up with neurology is important to monitor recovery and ensure another diagnosis (like multiple sclerosis) is not emerging.
When to Seek Help
- New neurological symptoms (weakness, numbness, confusion, severe headache, visual loss).
- Seizures or rapidly worsening alertness.
- Any concerning symptoms within 1–3 weeks after an infection.
Related Reading
- Another post-infectious immune disorder that affects the nerves rather than the brain: Guillain-Barré Syndrome.
- Examples of autoimmune conditions in other organs: Coeliac Disease and Graves–Basedow Disease.
Authoritative Resource
For detailed patient-friendly information, see the National Institute of Neurological Disorders and Stroke overview: NINDS: Acute Disseminated Encephalomyelitis (ADEM).
This article is for general information only and is not a substitute for professional medical advice. If you suspect ADEM or any neurological emergency, contact a clinician immediately.