Goodpasture’s Syndrome (Anti-GBM Disease)
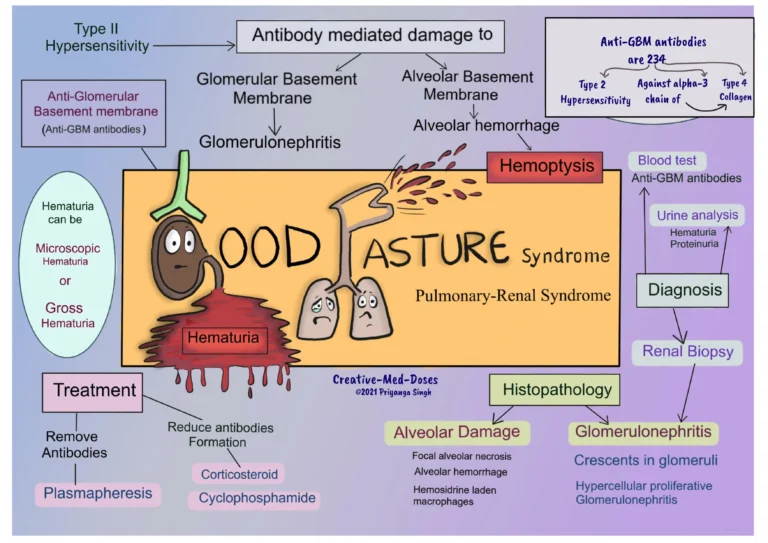
Goodpasture’s syndrome—also called anti–glomerular basement membrane (anti-GBM) disease—is a rare, rapidly progressive autoimmune illness in which antibodies target a collagen protein in the kidney glomerular basement membrane and the lung alveolar basement membrane. The result can be sudden kidney failure and life-threatening lung haemorrhage. Early recognition and urgent treatment are critical.
What’s Happening in the Body?
This is a classic type II hypersensitivity process: IgG autoantibodies bind linearly along the basement membrane of glomeruli and alveoli, triggering inflammation and tissue damage. Some patients are “double-positive,” with both anti-GBM antibodies and ANCA (anti-neutrophil cytoplasmic antibodies); these cases may have features of small-vessel vasculitis.
Who Is Affected & Triggers
- Very rare: roughly ~1 case per million people per year, with peaks in young adults and again in later adulthood.
- Smoking, recent lung infections, and exposure to hydrocarbons or metal fumes can precipitate lung haemorrhage in susceptible people.
- Certain genetic backgrounds (e.g., HLA-DR15) are associated with increased risk.
Signs & Symptoms
Lung involvement
- Dry cough, breathlessness, chest discomfort
- Haemoptysis (coughing up blood) ranging from streaks to massive bleeding
- Low oxygen levels; diffuse opacities on chest imaging
Kidney involvement
- Dark or bloody urine (haematuria), proteinuria
- Rapid rise in urea/creatinine with oliguria; ankle swelling, hypertension
- Fatigue, anorexia, nausea as renal failure develops
Red flags: new haemoptysis, rapidly worsening breathlessness, or sudden kidney dysfunction warrant immediate medical assessment.
How the Diagnosis Is Made
- Serologic testing: circulating anti-GBM antibodies (ELISA/reflective assays); check ANCA as well.
- Urinalysis & blood tests: haematuria, red cell casts, declining kidney function, anaemia.
- Imaging & bronchoscopy: diffuse alveolar haemorrhage pattern; bronchoalveolar lavage may show increasingly bloody aliquots.
- Kidney biopsy: confirms crescentic glomerulonephritis with linear IgG deposition on immunofluorescence—often the diagnostic gold standard.
Treatment (Urgent)
Prompt, coordinated therapy aims to remove pathogenic antibodies, halt new antibody formation, and support organs:
- Plasma exchange (PLEX) daily or on alternate days—typically for 2–3 weeks or until anti-GBM antibodies are undetectable.
- High-dose corticosteroids (e.g., IV methylprednisolone pulses followed by oral taper).
- Cytotoxic/biologic immunosuppression—commonly cyclophosphamide; rituximab is considered in selected scenarios or when cyclophosphamide is unsuitable.
- Supportive care: oxygen/ventilation for severe haemorrhage, blood transfusion as needed, and dialysis for renal failure.
- Smoking cessation and treatment of any concurrent lung infection to reduce recurrent bleeding.
Prognosis
- Lung recovery is often excellent once bleeding is controlled.
- Kidney outcome depends on severity at presentation (need for dialysis, degree of crescent formation). Some patients remain dialysis-dependent.
- Transplantation is feasible after disease quiescence; most centres require anti-GBM antibodies to be negative for at least 6 months to minimise recurrence risk.
Prevention & Follow-Up
- Strict avoidance of smoking and pulmonary irritants.
- Regular monitoring of kidney function and anti-GBM titres during and after therapy.
- Vaccination, infection risk counselling, and bone-health support while on immunosuppression.
Related Reading
If you’re exploring autoimmune and vascular conditions, you might also find these helpful:
- Antiphospholipid Syndrome — an autoimmune clotting disorder that can affect kidneys and lungs.
- Coeliac Disease — an autoimmune condition triggered by gluten that highlights how diverse autoimmunity can be.
- Guillain-Barré Syndrome — an acute autoimmune neuropathy often following infection.
Authoritative Resource
For a patient-friendly overview, see the National Institute of Diabetes and Digestive and Kidney Diseases: NIDDK: Goodpasture’s Syndrome.
This article is for general information only and is not a substitute for professional medical advice. Seek urgent care for coughing up blood or sudden kidney problems.