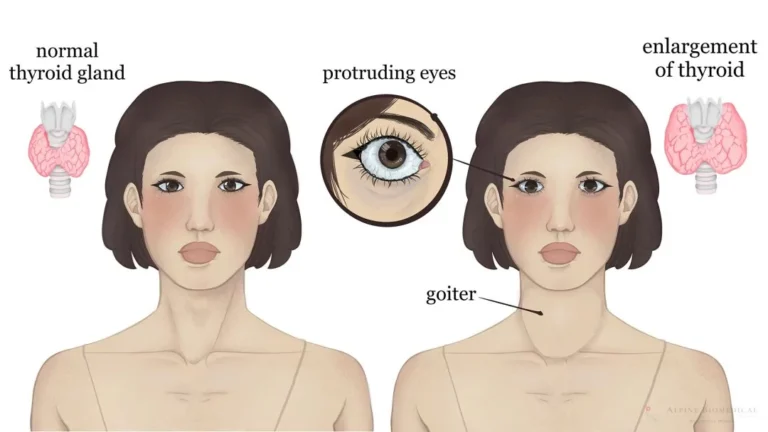
Graves–Basedow disease is an autoimmune thyroid disorder and the most common cause of hyperthyroidism. Antibodies stimulate the thyroid’s TSH receptor, driving excess thyroid hormone production. It predominantly affects women (about 8:1 vs men) and often presents in mid-adulthood. Because the same immune process can affect tissues around the eyes, thyroid eye disease (TED) may occur alongside thyroid symptoms.
Core Features
- Classic triad: hyperthyroidism, diffuse goiter, and eye signs (lid retraction, proptosis/exophthalmos).
- Systemic symptoms: heat intolerance, sweating, weight loss despite increased appetite, tremor, anxiety/irritability, fatigue, muscle weakness.
- Cardiovascular: palpitations, tachycardia, atrial fibrillation, widened pulse pressure; possible heart failure in severe/untreated cases.
- Dermatologic (less common): pretibial myxedema; thyroid acropachy (digital clubbing).
- Gastrointestinal: frequent stools/diarrhea; rarely vomiting.
- Eye disease (TED): lid lag, lid retraction, proptosis, periorbital swelling, chemosis; in severe cases, diplopia or optic neuropathy.
Emergency: an extreme, life-threatening exacerbation called thyroid storm can occur with infection, surgery, or other stressors—this requires urgent hospital care.
Why It Happens (Pathophysiology)
Autoantibodies (TRAb/TSI) bind and activate the TSH receptor on thyroid follicular cells, increasing hormone synthesis and release. Similar immune activity in orbital tissues contributes to eye manifestations. Genetic susceptibility (e.g., HLA-DR3) and environmental triggers (smoking, infections, stress) play roles.
Autoimmunity can involve multiple organs. For broader context, compare with other immune-mediated conditions like Coeliac disease or Crohn’s disease.
Diagnosis
- Labs: suppressed TSH with elevated free T4 and/or T3. TRAb (TSH-receptor antibodies) or TSI help confirm Graves’ disease.
- Imaging: radioactive iodine uptake scan shows diffuse increased uptake in typical cases; thyroid ultrasound evaluates structure and nodules.
- Eye assessment: clinical exam ± orbital imaging when moderate–severe TED is suspected.
Treatment Options
Choice depends on age, comorbidities, pregnancy plans, severity, and patient preference. Goals are to restore and maintain euthyroidism and to prevent complications.
1) Symptom control
- Beta-blockers (e.g., propranolol) for tremor, palpitations, and anxiety while definitive therapy takes effect.
2) Antithyroid drugs (ATDs)
- Methimazole/carbimazole are first-line for most adults; propylthiouracil (PTU) is preferred in the first trimester of pregnancy or for thyroid storm.
- Mechanism: inhibit thyroid peroxidase (organification/coupling); PTU also reduces peripheral T4→T3 conversion.
- Safety: rare but serious agranulocytosis—stop the drug and seek care urgently if fever or sore throat develops. Hepatotoxicity is uncommon but important.
3) Radioactive iodine (RAI) ablation
- Effective definitive therapy for many adults; induces hypothyroidism in most, requiring lifelong levothyroxine.
- Contraindicated in pregnancy and generally avoided with active, moderate–severe TED (can worsen eye disease; steroid prophylaxis may be considered in selected cases).
4) Surgery (thyroidectomy)
- Consider for very large goiters, compressive symptoms, suspicious nodules/cancer concern, poor ATD tolerance, or when rapid control is needed (e.g., in pregnancy when ATDs aren’t suitable).
- Risks: hypoparathyroidism, recurrent laryngeal nerve injury, bleeding.
Managing Thyroid Eye Disease (TED)
- Strict smoking cessation (smoking worsens TED).
- Lubricating drops/gel for exposure symptoms; selenium may help in mild active TED.
- For moderate–severe active TED: specialist-guided therapy (e.g., IV glucocorticoids); refractory cases may require orbital decompression or radiotherapy.
Pregnancy Considerations
- Use the lowest effective ATD dose to maintain maternal free T4 in the upper normal range; PTU is preferred in the first trimester, often switching to methimazole thereafter.
- RAI is contraindicated; surgery may be considered in the second trimester if needed.
Complications if Untreated
- Arrhythmias (especially atrial fibrillation), heart failure
- Osteoporosis and fractures with prolonged thyrotoxicosis
- Pregnancy complications (miscarriage, preterm birth)
- Thyroid storm (medical emergency)
Lifestyle & Follow-Up
- Stop smoking and limit eye irritants; protect eyes with sunglasses and lubricants.
- Prioritize sleep, balanced nutrition, and stress reduction—many find structured practices like this useful: How to Meditate – a Simple Meditation Technique.
- Regular monitoring of thyroid levels after starting treatment or changing dose; long-term follow-up to maintain euthyroidism.
Authoritative Resource
For patient-friendly, in-depth guidance, see the American Thyroid Association: ATA: Graves’ Disease.
This article offers general information and is not a substitute for personalized medical advice. Seek care promptly for severe eye pain, vision changes, chest pain, or signs of thyroid storm.