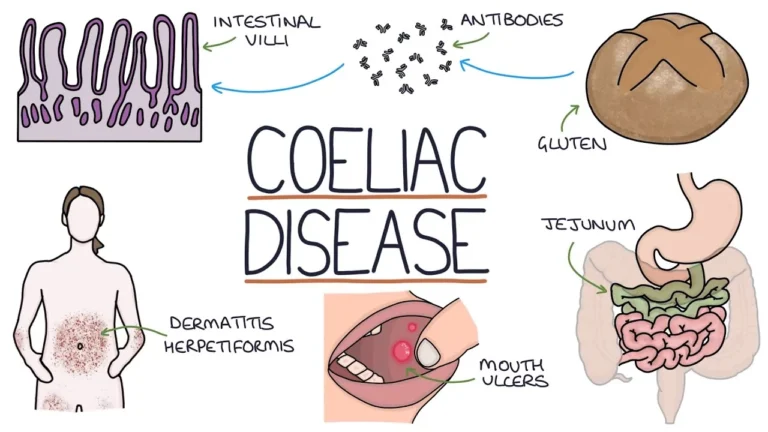
Coeliac disease is a chronic, immune-mediated enteropathy triggered by dietary gluten (proteins in wheat, barley, and rye). In genetically susceptible people, gluten exposure leads to inflammation of the small intestine with villous atrophy and crypt hyperplasia. This disrupts nutrient absorption and can cause gastrointestinal and non-gastrointestinal symptoms. With a strict gluten-free diet, the mucosa usually heals and long-term risks fall substantially.
Key Facts
- Affects roughly ~1% of the population (varies by region and ancestry).
- Can present at any age; many people have few or atypical symptoms.
- Associated with HLA-DQ2/DQ8 genetics and other autoimmune conditions (e.g., autoimmune thyroid disease).
Common Signs & Symptoms
Presentation is variable. Some individuals have classic GI symptoms, while others have extra-intestinal or silent disease:
- Gastrointestinal: chronic diarrhea or steatorrhea, bloating, excess gas, abdominal pain, nausea; some have constipation.
- Nutritional deficiencies: iron-deficiency anemia, folate or B12 deficiency, weight loss, fatigue, “brain fog.”
- Bone & dental: low bone density/osteoporosis (vitamin D/calcium malabsorption), enamel defects.
- Skin: dermatitis herpetiformis—an intensely itchy, blistering rash linked to gluten sensitivity.
- Neurologic/other: peripheral neuropathy, headache, reproductive issues (e.g., adverse pregnancy outcomes when untreated).
Symptoms overlap with other conditions such as irritable bowel syndrome and inflammatory bowel disease. For a comparison with a chronic inflammatory GI disorder, see Crohn’s disease.
Diagnosis
Do not start a gluten-free diet before testing, as it can normalize results and obscure the diagnosis.
- Serology: first-line is tissue transglutaminase IgA (tTG-IgA) with a total IgA level to check for IgA deficiency. If IgA deficient, use tTG-IgG or deamidated gliadin peptide (DGP) IgG. Endomysial antibody (EMA) IgA is highly specific.
- Upper endoscopy with duodenal biopsies: shows villous blunting/atrophy, crypt hyperplasia, and increased intraepithelial lymphocytes. Multiple biopsies improve sensitivity.
- Genetics: HLA-DQ2 and/or DQ8 are present in the vast majority of patients; absence makes coeliac disease very unlikely but is not diagnostic by itself.
Treatment
The cornerstone is a lifelong, strict gluten-free diet. This excludes wheat (including spelt, durum, einkorn), barley, and rye. Many tolerate pure, uncontaminated oats, but they should be introduced under clinical guidance and monitored for symptoms, as some react to oat avenin or to cross-contamination.
- Dietary support: referral to an experienced dietitian; education on label reading and cross-contamination (home and restaurants). For broader digestive wellness tips, see How Colon Care Promotes Colon Health.
- Micronutrient repletion: correct iron, folate, B12, vitamin D, calcium, and other deficiencies as needed.
- Monitoring: clinical review and serology (e.g., tTG-IgA) to track response; bone density assessment in adults at risk.
- Dermatitis herpetiformis: gluten-free diet plus, when required, medications (e.g., dapsone) under specialist care.
- Refractory coeliac disease: rare; persistent villous atrophy despite strict diet—requires specialist evaluation.
Prognosis & Long-Term Risks
Most patients experience symptom improvement within weeks of dietary change, with mucosal healing over months. Untreated disease raises risks of complications (e.g., osteoporosis, certain nutritional deficiencies). Historically there has been a small increased risk of specific intestinal lymphomas with longstanding, uncontrolled inflammation; risk lessens with strict dietary adherence and appropriate surveillance. For general information on prevention and screening principles, see our guide to cancer prevention and surveillance.
Who Else Should Be Tested?
- First-degree relatives of people with coeliac disease.
- Individuals with type 1 diabetes, autoimmune thyroid disease, Down or Turner syndromes, or unexplained iron-deficiency anemia.
- Those with persistent GI symptoms, low bone density, or unexplained neuropathy.
Living Gluten-Free
Adhering to the diet can be socially challenging, but availability and quality of gluten-free options have improved markedly. Planning, trusted brands, and clear communication at restaurants help maintain strict avoidance while keeping nutrition balanced.
Authoritative Resource
For comprehensive, patient-friendly guidance on testing, diet, and follow-up, see the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK): NIDDK – Celiac Disease.
This article is for general education and is not a substitute for personalized medical advice. Discuss testing and diet with your healthcare professional.